5-minute read | By Elizabeth Soltész, Registered Dietitian
Antibiotics Have Changed Our Lives—for Better and Worse
Access to antibiotics has revolutionized medicine. Once-deadly infections are now treatable, and dangerous complications from lingering illnesses can often be avoided. When antibiotics are truly needed—such as for pneumonia, strep throat, or urinary tract infections—it’s important not to delay treatment or rely on home remedies.
Equally important is taking the full prescribed course. Stopping early can lead to antibiotic-resistant bacteria, which are harder to treat. Unfortunately, many people take antibiotics for minor colds or simply to speed up recovery from viral infections—where they don’t help at all.
Treat antibiotics with care, just like fire. A well-tended fire keeps you warm and safe, but handled poorly, it can cause lasting harm.
Antibiotics Work, But at a Cost
The word “antibiotic” literally means “against life.” Interestingly, the idea for antibiotics originally came from nature—certain microbes, like fungi, naturally produce substances that kill bacteria to compete for survival.
Inside your body, your microbiome is a competitive ecosystem. Hundreds of types of bacteria, viruses, and fungi fight for space and resources. Modern antibiotics, however, aren’t selective enough. While they kill harmful bacteria, they also wipe out many of the beneficial bacteria in your gut, drastically changing your internal balance.
Long-Term Support for Your Microbiome: The Power of Prebiotic Fibers
A diverse gut microbiome is one of the most important pillars of long-term health. Unfortunately, medications and unhealthy lifestyle choices can reduce this diversity quickly—rebuilding it takes time and effort. So how can you strengthen your microbiome to withstand unavoidable antibiotic treatments?
Supporting your microbiome isn’t a short-term fix—it’s a lifelong commitment and an essential part of self-care. Your good bacteria rely on you to feed them with prebiotic fibers, their main source of fuel.
To nourish them:
-
Eat a wide variety of plant-based foods at every meal: vegetables, raw greens, legumes, whole grains, seeds, and nuts.
-
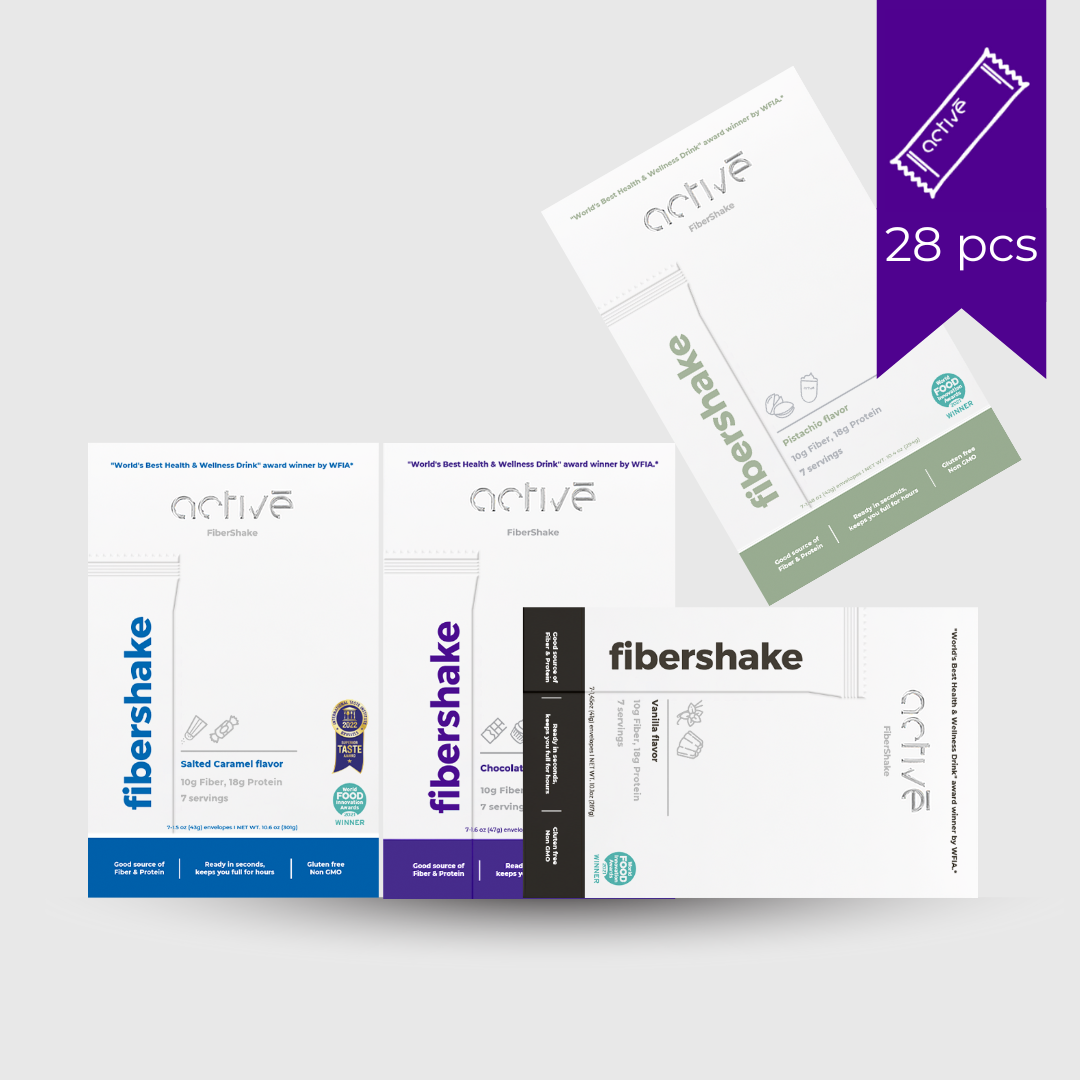
If you choose a prebiotic fiber supplement or drink, opt for one made from natural ingredients, free from artificial sweeteners and additives.

Temporary Disruptions During Antibiotic Use
Even with a fiber-rich diet, your gut may still struggle temporarily during antibiotic treatment. Why?
Normally, your microbiome ferments dead intestinal cells and dietary fibers—this process produces short-chain fatty acids (SCFAs), which not only feed your good bacteria but also help maintain hydration and electrolyte balance in your colon.
Antibiotics reduce the population of fiber-fermenting bacteria, slowing down digestion and disrupting water and mineral absorption—leading to diarrhea. They also allow normally suppressed harmful microbes to flourish, causing excess gas and inflammation, which can further worsen diarrhea. These symptoms often linger after you finish the antibiotics, as your microbiome takes time to recover.
The Long-Term Impact
It’s almost inevitable that antibiotics will temporarily disrupt your microbiome. A healthy adult microbiome is usually resilient, able to recover with the right diet and lifestyle support.
However, frequent or long-term antibiotic use, especially at a young age, can have more serious, lasting effects. If your microbiome was already unbalanced before treatment, the recovery may be slower—even for adults.
Studies show that antibiotic use can permanently reduce microbial diversity, alter the balance of metabolism-regulating bacteria, and decrease the production of gut-protective fatty acids.
These shifts have been linked to increased risks of obesity, metabolic disorders, inflammatory diseases, and autoimmune conditions. Disruptions to the gut-brain axis, a sensitive biochemical communication system, may also contribute to higher rates of anxiety and depression.
Probiotics and Prebiotic Fibers: Natural Allies
Probiotic bacteria support your health in many ways. Common types like Lactobacillus and Bifidobacterium are especially important early in life but remain beneficial throughout adulthood.
They help suppress harmful bacteria, maintain a healthy gut lining, support immune function, regulate digestion, and produce nutrients for gut cells.
Given their benefits, it’s wise to help replenish your good bacteria after antibiotics. You can take over-the-counter probiotic supplements and boost your diet with probiotic-rich foods like yogurt, kefir, and fermented vegetables (e.g., sauerkraut, pickles, kimchi). Ideally, these foods should be a regular part of your diet.
For effective microbiome support, daily prebiotic fiber is also essential. These fibers are the primary food source for probiotics. You can get them from vegetables, legumes, fruits, and whole grains—or add a quality fiber supplement for extra support.

Probiotics and Antibiotics: Always Take Them Together
Probiotics are always recommended during antibiotic treatment. While a single dose won’t fully restore your gut flora, regular use improves your odds. Everyone’s microbiome is unique, so the impact of antibiotics—and the effectiveness of any given probiotic—can vary.
During antibiotic treatment, probiotics help crowd out harmful bacteria, strengthen immune responses in your gut, and produce compounds that support long-term recovery. Choose products with at least 5-10 strains of probiotic bacteria and a high potency (aim for 10⁹ CFUs or more).
Start taking probiotics on the first day of your antibiotics (or even at the onset of symptoms), and time them at least 2 hours apart from your medication for best results. You can eat prebiotic-rich foods throughout the day.